Light Heart
Bringing the power of an ECG to smart phones.
Website
Status
Archived

Context
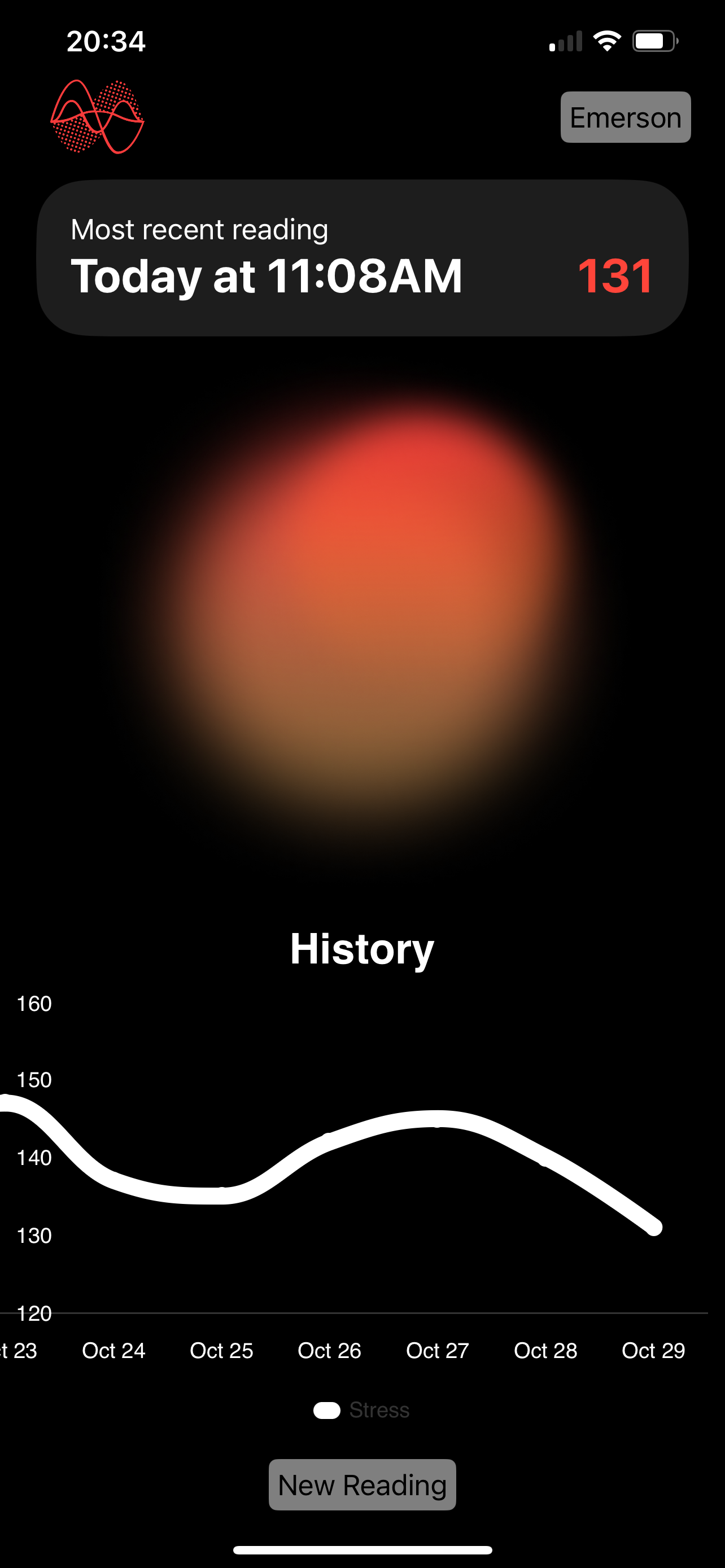
Light Heart was a product built during my time at CoreHealth. I spearheaded the research, development, and testing of its algorithms and oversaw the app’s design. The main motivation for its development stemmed from the reality that despite high rates of stress and anxiety — according to a 2023 Deloitte survey, 77% of respondents reported experiencing burnout [1], and the ADAA estimates that approximately 19% of the U.S. population is affected by anxiety [2] — there doesn’t really exist a single comprehensive way to measure either.
We achieved something close shortly after CoreHealth was acquired. Further details can be found in the validation study published in partnership with researchers at Brock University: “Examining the Light Heart Mobile Device App for Assessing Human Pulse Interval and Heart Rate Variability: Validation Study” [3].

The physiology behind Light Heart
Light Heart used a reading of heart rate variability (HRV) to approximate users level of stress. HRV represents the variation in time between consecutive heartbeats and indicates the autonomic nervous system’s regulation of heart rate, reflecting the dynamic interplay between the sympathetic (fight or flight) and parasympathetic (rest and digest) nervous systems.
Being able to capture HRV by smartphone was a good foundation, but the challenge with using HRV to estimate mental stress is that, while validated as a general stress measure, it’s also affected by physical activity. To isolate mental stress, Light Heart proposed a twofold approach. We developed a proprietary adaptation of Baevsky’s stress index — a well-recognized HRV-based stress assessment [4] — and aimed to incorporate physical monitoring tools (HealthKit, Apple, and Garmin watches) to control for physical stressors in our model.
Photoplethysmography (PPG)
To actually perform the HRV reading, we employed an adapted photoplethysmography (PPG) method to perform HRV readings. PPG measures blood volume changes by tracking light intensity shifts. With a fingertip placed on the smartphone camera, Light Heart was able to capture and quantify these slight fluctuations.
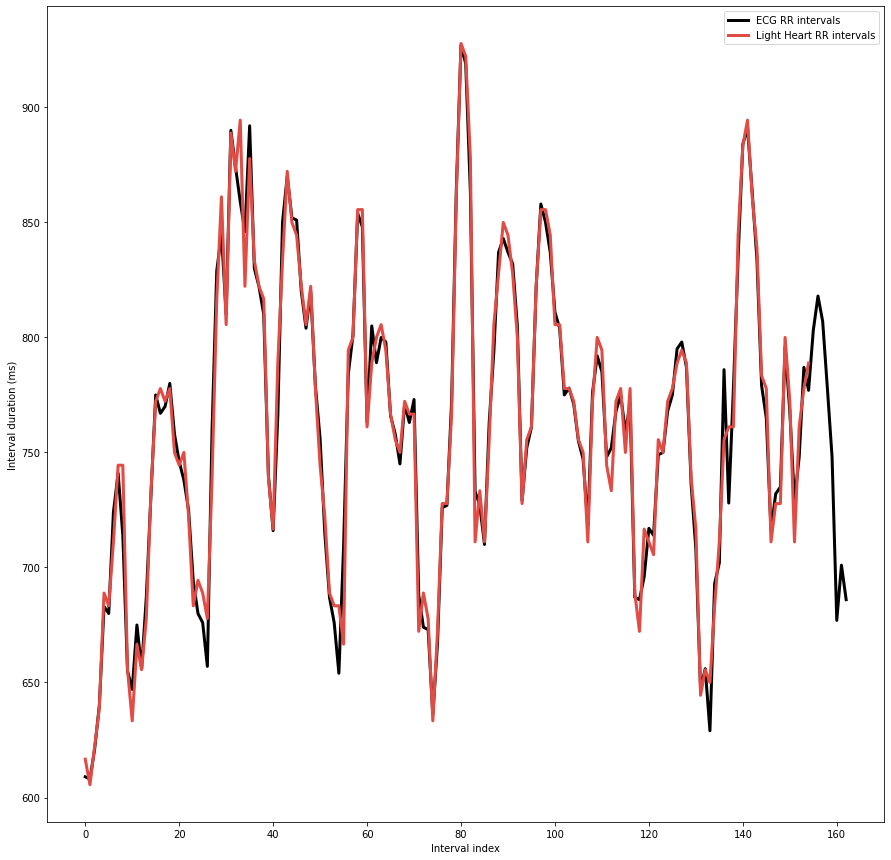
Figure demonstrates an average absolute error of ~7 ms between Light Heart and an ECG - a shorter amount of time than a blink.
Architecture & techniques
Since some of the algorithms are proprietary, here’s a brief overview: a reading was taken by recording the fingertip at 30 FPS for one minute using the phone’s torch as the light source. Light Heart conducted on-device image processing in Swift, calculating average RGB values for each frame and converting them to HSL (Hue, Saturation, Luminosity) to use luminosity as a proxy for intensity.
This array of luminosity values was then sent to an Azure server for further processing—smoothing, filtering, and noise reduction. Afterward, the signal was interpolated to correct any gaps from movement artifacts, and the HRV metrics and stress index were computed and sent back to the phone. Although the goal was to eventually perform all processing on-device, for testing, debugging, and study purposes, we opted to handle the more complex processing off-device.
During the reading, Light Heart continuously monitored signal quality, confirming the signal through RGB values and assessing the luminosity stability by performing an Fast Fourier Transform (FFT) and monitoring in the frequency domain, the intuition being that a signal without much noise should have a single dominant frequency.
[1] https://www2.deloitte.com/us/en/pages/about-deloitte/articles/burnout-survey.html
[2] https://adaa.org/understanding-anxiety/facts-statistics
[3] Klassen S, Jabbar J, Osborne J, Iannarelli N, Kirby E, O’Leary D, Locke S Examining the Light Heart Mobile Device App for Assessing Human Pulse Interval and Heart Rate Variability: Validation Study JMIR Form Res 2024;8:e56921 URL: https://formative.jmir.org/2024/1/e56921 DOI: 10.2196/56921
[4] Roman M. Baevsky, Anna G. Chernikova. Heart rate variability analysis: physiological foundations and main methods; Cardiometry; No.10 May 2017; p.66-76; DOI: 10.12710/cardiometry.2017.6676 Available from: www.cardiometry.net/issues/no10may-2017/heart-rate-variability-analysis